I first met Li in February 2005 at a conference table with a great breast cancer support group. The group was for early stage breast cancer and everyone in the group that day were all in the middle of chemotherapy while I was about to start my first round of adriamiacin and cytoxin. I had to do chemo because they found the cancer in my first lymph node. I had no problem undergoing a surgical lumpectomy, sentinel node biopsy, or axillary dissection, but when I heard I needed to do chemotherapy and I would lose my hair, I knew I needed some help.
It was ironic that in November my hair stylist of several years chopped my hair very short when I asked her for a little trim. I was furious that my long hair was gone, so I went and got hair extensions until my hair grew longer again. I told the group I had extensions and Li picked up immediately that I was not going to do well losing my hair.
 The next time I saw Li was in my oncologist’s office when I was about to leave. As I looked up from my papers she came out into the waiting room. I saw her and immediately gave her a huge hug and realized she went to the same office with a different oncologist.
The next time I saw Li was in my oncologist’s office when I was about to leave. As I looked up from my papers she came out into the waiting room. I saw her and immediately gave her a huge hug and realized she went to the same office with a different oncologist.
Since she was alone I asked her how she was getting home and she said she was going to call a cab. Li lived in Santa Monica near the oncology office and managed to get around by bus, friend’s rides or taxis. I offered her a ride in my car parked far away. As we walked she was getting out of breath, because her red cells were very low from the chemo, but I kept telling her we were close to the car.
We started calling each other and found that we had a lot in common. I had a graphics arts background with a degree in architecture and she had worked as a designer at the Smithsonian. She left her job taking a very early pension and after seeing the Pentagon in flames from her apartment window on 911. She moved back to California where she and her ex-husband had lived before she went to DC.
The day my hair fell out we spent the day on the phone talking for hours. She was so supportive since she knew this was something I was not comfortable with at all. From that day forward we spoke with each other practically every day, and it was so comforting for both of us going through chemo together. Her regimen was adriamyacin every 3 weeks for 6 rounds totaling 18 weeks of treatment. Mine was “dose-dense” adriamyacin and cytoxin every two weeks for four weeks, followed with taxol every two weeks for four weeks totaling 16 weeks of chemo.
We talked about breast cancer and chemobrain plus our lives, side effects, research and managing to get through treatment, and we thought we knew a lot about breast cancer. We went out for meals together and one of our favorite places to eat was a Chinese restaurant run by a family we called “Lucy’s”, since Lucy always served us while her mother was in the kitchen. We both had terrible stomach issues during chemo. I had trouble keeping any food down and her food just seemed to run out of her little body.
We became extremely close because we were experiencing the same “trauma” at the same time. We would lose ourselves in conversations and never missed a Saturday to get together. We could both talk without our wigs on and I laughed when she made fun of me for holding on to whatever strands of hair would stay on my head. Truthfully, I did look a little bizarre with 20 stands of knotted up blonde hair and probably should have just had my head shaved!
She also helped me through the crying jags since my hormones were going crazy. When one of my front crowns kept falling out, she made me laugh at myself being bald and toothless as I would call the dentist to glue the tooth in one more time till I finished treatment and could take care of the tooth properly.
We both needed surgeries and we never missed being the person to go with each other for surgeries. Li also got a dog named Shelby who is part shih-tzu and part maltese. Li had moved from a studio to a one bedroom so she could have more room and be able to take care of Shelby. She bought puppy gates and it was so much fun to visit her with Shelby, who I fell in love with from the day I saw her fitting in the palms of Li’s hands.
When Li had some cysts that she was not sure were cancerous she had an oophorectomy. Fortunately they were not cancer. She woke up crying which was so unusual for her. I think her mind knew that her female plumbing was missing and her tears were her hormones and her mind realizing that her breast and her ovaries etc. were missing.
In February 2007, I had a recurrence in the same breast, which my breast surgeon said had to have a mastectomy. I had finished treatment a year and a quarter earlier and had several biopsies that were false alarms in both breasts. My breast surgeon handed me business cards of plastic surgeons that he worked with.
The first surgeon saw me right away and it turned out he did Li’s reconstruction when she had her mastectomy and her results were awful. He wanted to do a Diep Flap (taking the tissue from my tummy and putting it in my breast). He also wanted $30,000.00 dollars over my co pays with my insurance to do the procedure. I ended up picking the plastic surgeon that accepted my insurance, but that decision left me with many extra surgeries because I had a radiated breast that caused multiple surgical failures.
Like every other surgery, when I had the bilateral mastectomy surgery, Li was with me. I encouraged her to go back to the first surgeon and get him to fix her botched job. She had her surgery after mine and when I went to talk to her doctor the first thing he said to me was “It’s very hard for a woman to lose her breasts”. I could not believe he didn’t recognize that I was in his office only two months before Li’s surgery. I said “Tell me about it . I have had a bilateral mastectomy with reconstruction”. The next thing he said was that Li’s insurance probably wouldn’t pay for her stay that night. I explained she had a pre-approval letter and let him know that I saw him for a consult making him have to say he remembered me even though he didn’t. Awkward!
I knew how organized Li was with her paperwork, so when I went to her hospital room after speaking with her surgeon. Li pointed me to the paper with the pre-approval from her insurance. I called her insurance right from the hospital to make sure they were covering her hospital stay for the night. The plastic surgeon was wrong.
The next morning, Li had trouble breathing and she felt very out of sorts. We called the nurse who got hold of her Doctor. He said “When I did the surgery I may have kind of sort of nicked her lung”. I asked him, “In what percentage of patients does this occur”? He replied, “only her”. I asked what they were going to do about it and he told me they would do a surgical procedure right in her hospital room by surgically placing a large tube in her side to build her collapsing lung back up. I couldn’t resist asking, “Are you sure her insurance will cover her to stay at the hospital longer after the procedure”? Of course the answer was yes, and I am so glad Li knew to get approval to stay overnight for her procedure, because if she had gone home and her lung collapsed I don’t want to think about how that would have gone down.
I stayed with my friend Li to hold her hand as long as I could while they prepped her for the surgery. They told me I had to leave the room while they did the surgery or I might faint. They don’t know me. I am very good in hospitals and I can handle blood and surgery.
When I needed my tissue expanders out and got my first implants, Li was with me. That surgery eventually failed. After my recurrence I was very beaten down and I really wanted to spend some time with my family living in Tennessee. I ended up selling my LA condo and moved part-time to Nashville so I could be closer to them. But I kept my doctors and especially my oncologist in LA. I was lucky that another great friend in the group of 8 women breast cancer survivors (that now met at each other’s houses), rented a room to me in LA, so I could travel back and forth.
In February 2009, I flew to LA for the monthly group meeting and hung out with Li for most of the time like we always did when I came to LA. We would go together to doctor appointments, restaurants, meetings and I also would bring my computer over and get work done while she did her work since she had wifi. She looked the healthiest I had ever seen her. She had gained some weight and her hair looked so beautiful and healthy. I told her how awesome she looked and we were so glad we made it through all that treatment. Li mentioned the last time she saw her oncologist she was told that it was a great sign that she was 4 1/2 years out with her pathology.
She was supposed to have her appointment with her oncologist when I was there and we were going to go together, but her oncologist had to change it, so Li changed the appointment for her birthday on February 19th. Li told me she had a small rash on her breast that she thought her bra must have caused. We both ate very well as we were enjoying the fact that our stomachs were returning to a new normal.
I returned to Tennessee and I called her later in the day on February 19th to wish her a Happy Birthday, assuming her oncology appointment went well since she looked so healthy. Li was a mess. She said that her doctor sent her to her breast surgeon for an immediate biopsy and the look on her doctor’s face made her feel like this was extremely serious. It was. The rash was skin legions from Metastatic Breast Cancer (MBC) and she also had it in her bones. She was Stage IV and had to start chemo again right away.
I ended up moving back to LA permanently in July 2011. I was very glad that I could be with Li so much during the last seven months of her life.
Li’s strength, courage and determination throughout her treatment were amazing. I felt awful especially thinking back to the day when we were going through primary treatment and she was going to have what I thought was her last chemo the next day. We were together in front of our favorite restaurant “Lucy’s” in Santa Monica. Li’s red cells were awful so she had to sit down on a bench. I said to her “Li this is the last chemo you will ever have to do again in your life”. Sadly I was wrong.
Li worked very hard putting her affairs in order before the cancer traveled too far for her to have treatment anymore. As soon as she was sick with MBC she asked me if I would take care of her dog Shelby. I said, “of course” yet I hoped she was around for a very long time to enjoy the joy that Shelby brings. I remember when she was getting close to the end and I asked her if she was afraid. She said, “I’m not afraid of death but it’s the indignity of all of it that bothers me.” I knew that losing her mobility and not being able to do things for herself plus ending up thin, bald, and with a huge stomach from her liver metastasis building up fluid was no picnic. Luckily we found the most wonderful caretaker, Cora, who Li and I adored. She was such a comfort to Li constantly cleaning and making Li’s home beautiful plus running any errands Li needed done.
A few days before she died the caretaker Cora, Li and I had dinner. Li sat up in her hospital bed that we had in her room at home while Cora and I sat in chairs surrounding her. I said, “Li remember when we first went through chemo and we thought we knew so much about breast cancer? Boy were we wrong”. Li and I just laughed. We were trying to be normal having dinner, but truthfully there was nothing normal about anything that was going on. Li was getting more tired and going from moments of extreme clarity to moments of disorientation and confusion.
The last night of her life I came to join Li for dinner and she was particularly tired and didn’t feel like eating. I held her hand for some time while she went in and out of sleep. She said to me “I always love when you come by for dinner”. I told her that I loved her and was so grateful for our friendship, which I said at the end of so many of our conversations. She said she loved me too and went back to sleep.
She died that night and I received the call from another great friend who had also been by Li’s side through this daunting process. Li donated her body to science and did not want a funeral. When they came to get her body for UCLA, I was so impressed by how dignified they wrapped her up in a beautiful white sheet.
Since I promised her I would take care of her dog Shelby, I took Shelby and all of her things back to my home that day. I miss my friend a lot. Thanks to her incredible gift of Shelby I feel Li’s presence every day.
Li’s death from MBC along with the friends I know who have cancer that has metastasized has made me determined to make an impact on seeing that we have an end to this disease.
I know that 1 in 8 women will get breast cancer in their lifetime and 109 women in the US die a day from breast cancer. (I haven’t forgotten that there are also men that get breast cancer too). This means one death every 14 minutes. With each person there is an important story.
I feel guilty sometimes that it wasn’t me instead of Li. It still could be me. That’s what is so cruel about the disease. We think we know so much more about the disease, but when it comes to the loss of lives we haven’t made much progress. True we can keep someone alive longer with chemotherapy drugs, but eventually cruel cancer figures out a way to outsmart the drugs so they no longer work.
My fearless friend Li, was not just another statistic. We had an incredible bond as a result of breast cancer and we cemented our friendship with being supportive of each other as breast cancer was always with us.
I know her spirit lives on through the memories of her. I especially get comfort every day from Shelby. I am truly lucky that I got to know Li and I treasure the time that we got to spend together.
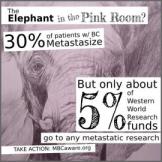 I have written about my passion (see: While Flying – Frustration surrounds Me ) for doing everything I can to advocate for Metastatic Breast Cancer (MBC). 6-10% of breast cancer patients are initially diagnosed at Stage IV (MBC). 30% of all breast cancer patients initially diagnosed with early stage breast cancer will eventually metastasize (or have what some of us call mets).
I have written about my passion (see: While Flying – Frustration surrounds Me ) for doing everything I can to advocate for Metastatic Breast Cancer (MBC). 6-10% of breast cancer patients are initially diagnosed at Stage IV (MBC). 30% of all breast cancer patients initially diagnosed with early stage breast cancer will eventually metastasize (or have what some of us call mets).  As an update to A4BC, we are in the process of getting our official site up and we are working around the clock to have it done. We are now on Facebook. Thank you everyone for liking the page and if you haven’t seen it, please have a look and “like” the page to stay updated. Please click on: https://www.facebook.com/advocates4breastcancer.
As an update to A4BC, we are in the process of getting our official site up and we are working around the clock to have it done. We are now on Facebook. Thank you everyone for liking the page and if you haven’t seen it, please have a look and “like” the page to stay updated. Please click on: https://www.facebook.com/advocates4breastcancer.